Executive Summary
Formed in 2010 by a widely respected private equity firm, Atlantic Medical Management (AAM) concentrates on finding ways to overcome the barriers posed by value-based payment models in order to help independent practices stay independent, improve patient care, and earn appropriate financial rewards for physicians and owners. It focuses on improving quality, enhancing revenues and reducing system costs.
Several years ago AMM identified Jacksonville Children’s and Multi-Specialty Clinic (JCMC) as a unique physician practice. In order to fulfill its mission to “serve our patients, support our providers, empower our people and value our payers,” AMM partnered with JCMC to enjoy the synergy of both organizations’ strengths.
JCMC’s journey to becoming a model physician group began with a familiar challenge: In today’s fast changing regulatory and payment environment, mid-sized and even many large independent physician groups struggle to simultaneously reduce costs and increase revenue, without sacrificing quality and patient experience.

The 40-provider group had grown steadily for three decades, serving a high proportion of Medicare and Medicaid patients across seven rural counties, as well as the military families of Camp Lejeune and New River Air Station. But the accelerating shift to value-based care—especially pronounced in Medicare and Medicaid— threatened JCMC’s future. The group’s leaders knew they would have to rethink their strategy to transition and continue to grow under value-based care.
Their solution: leveraging technology and process transformation to improve the revenue cycle without sacrificing high-quality clinical care or patient satisfaction. Several years in the making, the new approach has made JCMC a model of innovation and high performance among North Carolina physician groups.
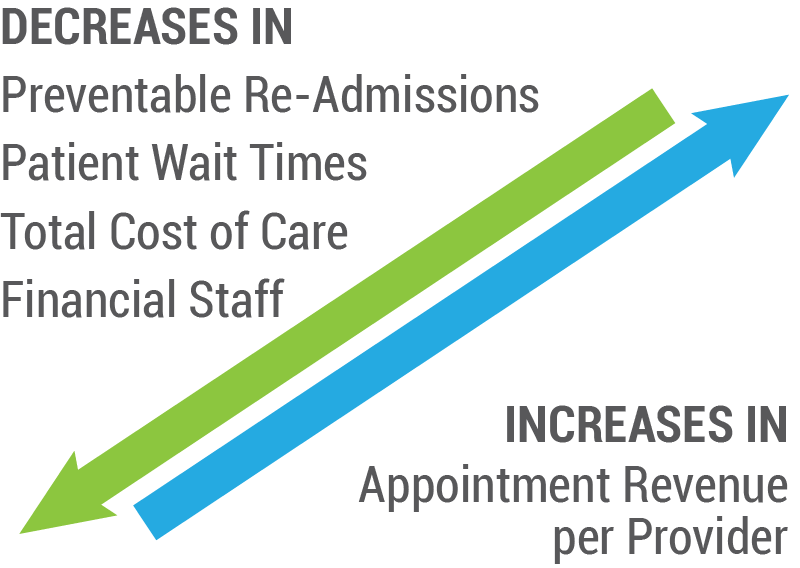
RESULTS:
• 25% below the regional average in total cost of care
• 75% below the regional average in preventable readmissions
• 32% increase in revenue with 15% rise in appointments per provider
• 50% reduction in financial staff (most reassigned to more productive roles)
• 75% improvement in patient wait times (from 20 minutes to 5 minutes)
Rise of Value-Based Care Poses New Challenges
“As the movement away from fee-for-service accelerated, we knew we would have to focus on improving quality while lowering costs, and without negatively impacting our patients.”
-Madhur Mittal, MD
President and Chief Medical Officer of JCMC
Small and mid-sized physician practices across the country often struggle to remain financially viable in the face of falling reimbursement rates and related market trends. Rising administrative burdens add to the pressure. New requirements from employers, insurers, and government are difficult to manage and require ever-increasing investments in the infrastructure needed to grow revenue as well as collect, manage and report data.
The pace of change has been especially fast in government-funded health programs. In 2015, the Centers for Medicare and Medicaid Services (CMS) announced its goal of tying 50 percent of Medicare payments to quality or value through alternative payment models by the end of 2018. Many states have followed CMS’s lead by adopting value-based payment (VBP) programs for Medicaid. In 2015, the North Carolina General Assembly enacted legislation to transition Medicaid and NC Health Choice from fee-for-service to managed care, with a strong VBP focus. Major North Carolina health systems have followed suit, signing VBP agreements across multiple payers, despite the political deadlock that has delayed enactment of Medicaid Transformation.
Leaders at JCMC saw the change coming two years before the state approved Medicaid Transformation. In 2013, the group launched a plan to make JCMC a value-based care leader. The strategy hinged on accomplishing four potentially conflicting goals: increasing revenue, lowering costs, improving quality and maintaining or improving the patient experience.
As the movement away from fee-for-service accelerated, we knew we would have to focus on improving quality while lowering costs, and without negatively impacting our patients,” said Madhur Mittal, MD, President and Chief Medical Officer of JCMC. “We knew accomplishing that wouldn’t be easy, but it was the only way to succeed under value-based care while continuing to help the community and our patients.”
The Path Forward: Quality Certification + Technology Innovation
Becoming a value-based care leader would require a multi-pronged effort. JCMC began by undertaking the rigorous process of becoming NCQA certified as a Level 3 Patient-Centered Medical Home (PCMH), a model of care that puts patients at the center of care. With NCQA certification in the hat, in 2014 JCMC was designated by Blue Cross NC as a Level 3 Blue Quality Physician Program (BQPP) participant, able to earn rewards for providing high-quality, low-cost, and patient-centered care.
Not yet satisfied with the group’s level of preparation for value-based care, in 2016 JCMC’s leaders launched the rigorous improvement process known as Practice Transformation. The process takes PCMH to the next level, requiring not only basic PCMH certification, but also implementation and optimization of an electronic health record (EHR), as well as quality-improvement activities such as population health management and reducing barriers to care.
In concert with its practice transformation initiative, JCMC continued its long-held practice of exploring technology innovations that would support operational improvements and value-based care. For example, JCMC’s IT team developed a program that analyzed patient data within the group’s NextGen EHR to uncover clinical gaps in care – a key focus for population health management programs. The initiative ended up driving more revenue to the group while also improving quality.
“We can run a report on a specific protocol, such as when was the last time they had a physical, and it will pull data from NextGen to give us a list of 500 patients who need physicals,” said Jessica Brackett, JCMC’s Director of Revenue Cycle Management. “Then our receptionist staff starts making calls to get those patients in here for their physical.”
Around this time, JCMC launched a series of additional technology initiatives designed to improve patient satisfaction and streamline participation in value-based care programs:
• EHR customization to automate reporting of quality data to ACOs and other entities
• A patient portal enabling access to medical records, appointment scheduling, and caregiver messaging
• Point-of-care electronic patient surveys to gather patient feedback and drive improvement in service
• EHR-Lab interfaces with Meditech, Lab-Corp, and Quest
• Automatic notifications when patients visit outside facilities via NC Notify (North Carolina Health Information Exchange)
• Bi-directional document and lab interfaces with other North Carolina providers on the Coastal Connect Health Information Exchange
• Robotic insertion of immunization data from the North Carolina Immunization Registry directly into JCMC’s EHR (via Smartlink Health)
• Electronic referrals to high-performing providers to support care coordination (via Infina Connect)
• Pre-arrival focused patient intake and registration to reduce patient check-in times (via Yosi Health)
Taken together, these substantial new capabilities enabled JCMC to meet—and in many cases to automate—key requirements of value-based contracting such as reporting quality metrics and providing comprehensive care management.
Pushing Revenue Cycle to New Heights Through Collaboration
REVENUE CYCLE SUCCESSES
• Reduced RCM staff from 15 people to 8 (while revenue increased by 32%)
• Achieved a clean claim rate of 97% versus the US hospital average of 75% to 85%
While technology plays a key role in JCMC’s success, equally impactful are the process improvements the group has put in place. The changes are most evident in the finance department, where new hires with deep experience in revenue cycle management, compliance and revenue integrity have transformed JCMC’s back-office operations.
Brackett came to JCMC in 2018 after several years in patient financial services for one of North Carolina’s largest health systems. Expecting to find that the group’s financial practices were lagging those of the health system she was instead pleasantly surprised. “Working in a large health system, you assume that everything is well-oiled and working smoothly. But when I got here I was like, ‘hmm, I guess they weren’t as well-oiled as I thought,’” Brackett said.
Despite her initial surprise at JCMC’s smooth operations, Brackett soon found that the organization provided new opportunities for improvement that would have been unthinkable in a large health system. In particular, JCMC’s providers, rather than being shut out of the RCM process as Brackett had come to expect of health system providers, were eager to help improve the group’s financial practices.
“They wanted to know how well they were doing with coding. They wanted to get advice on how to do better at their job to improve revenue. So it has become a very collaborative process,” Jessica Brackett said.
The most compelling evidence of the collaboration between finance and clinical is JCMC’s ability to increase revenue by 32% in 2019 while increasing the patient load per provider by just 15%. Rather than drive new revenue through the tried-and-true method of overloading providers and risking burnout, JCMC boosted revenue largely by revamping its coding and RCM practices.
New processes initiated by JCMC that contributed to the group’s success include automation of payer contracting to clarify actual collectible revenue versus an adjustment that will eventually be written off or a mistaken balance. Knowing the exact payment the group should expect from payers and from patients every time has enabled JCMC to reduce days in accounts receivable from over 30 to 11 days or less.
Other outcomes of the movement toward automation of the revenue cycle include:
• Reduced RCM staff by almost half, from 15 people to eight (while revenue increased by 32%)
• Achieved a clean claim rate of 97% versus the US hospital average of 75% to 85%. Submitting clean claims is critical to reducing claim denial rates, getting paid, and improving the revenue cycle.
• Lowered the average time between provider documentation of an encounter to billing the encounter from 10 days to between 3 and 6 days.
Revenue Integrity Program Ensures Stability
“The stability of a practice is strongly dependent on ensuring that you’re doing things in a way that puts you out of harm’s way”
-Zen Menon, CEO of JCMC
Another key addition to JCMC’s financial leadership team was Chief Compliance Officer Mike Runquist. A veteran of large-scale revenue integrity initiatives at Blue Cross Blue Shield of Washington, as well as the University of Washington’s physician group, Runquist is an expert in healthcare compliance issues. Few mid-sized physician groups invest in developing a full revenue integrity program. But JCMC’s CEO Zen Menon, was convinced that the program would drive the group’s financial performance while limiting the risk of failing to comply with the vast array of government and payer rules regulating medical billing and collections.
“The stability of a practice is strongly dependent on ensuring that you’re doing things in a way that puts you out of harm’s way,” said Menon. “Many medical practices view revenue integrity as reactive, something you do only if a (claim) denial is tied to a change in regulations. But you need to be on top of it before a denial and before an audit. As practices grow, they need to prioritize managing what will kill their practice overnight.”
The goal of JCMC’s revenue integrity program is to reduce compliance risk and avoid revenue leakage. Runquist’s team reviews and monitors the revenue cycle process from beginning to end to identify and correct issues that could lead to missed revenue. The team also reviews billing, coding, and other processes to make sure the group is billing, and being paid, according to its payer contracts. And they review JCMC’s referral relationships, physician arrangements, and contracts to make sure the group isn’t at risk for violating any Stark law (self-referral) or Anti-kickback statutes.
The team discovered that JCMC’s providers were overlooking revenue opportunities on a daily basis. One common example, said Runquist, is when a patient is seen for a preventive medicine service and their provider ends up treating an acute or chronic problem that the patient presents with. This could be as simple as diaper rash, or as complex as jaundice, or virtually any problem requiring a diagnostic test. In that case, the preventive visit could be billed as an additional office visit since the provider had separately identified a problem that was unrelated to the preventive service visit.
JCMC’s revenue integrity program is akin to an internal auditor of the group’s entire revenue generation cycle, said Runquist. “We look at physician productivity to determine how many patients they’re seeing, how long they’re spending with patients, how much they’re billing, and to identify any issues with productivity. Whether it’s the process of scheduling or pre-authorizations, we provide oversight on the whole cycle to see if there are issues we can tighten up to avoid missing revenue, and also collecting more than we should.”
Technology Innovation Expands Patient Care Access & Engagement
Complementing JCMC’s success with the revenue cycle, the group’s integrated technology and process transformation have also delivered meaningful improvements in clinical quality and patient satisfaction. This is due in no small part to the prioritization of creating broad access for patients. For example, JCMC offers same-day access across the enterprise as well as Saturday and Sunday hours on the main campus. Additionally, JCMC started an urgent care center–open from 10 a.m. to 8 p.m. seven days a week for all JCMC patients–weekend pediatric sick clinics, and on-call providers that are available 24×7 year-round. JCMC also ensures through patient education that patients are well aware of these new ways to garner care. Furthermore, JCMC monitors access data including appointment and patient survey feedback, and has seen increasing utilization of these convenient, cost-effective care options.
The flip side of physical patient access is digital access. Joining efforts with technology partners Yosi and Smartlink Health Solutions, JCMC launched digital patient intake and registration, patient scheduling and bill pay via tablets, enabling fast, electronic updates to medical history, insurance information and more–all of which is then transmitted seamlessly to the EHR. This digital transformation—the first of its kind for NextGen EHR users nationwide—has reduced typical patient wait times by 75 percent, from 20 minutes to 5 minutes. From the provider’s perspective, she or he can instantly see the patient’s diagnosis and medications versus wasting precious time reviewing paperwork. After an office visit, patients can log into the patient portal to review their medical records, lab test results, scheduled appointments and even communicate with their providers, extending their access to patient care tools while boosting patient and provider engagement.
Comprehensive Care Management Enhances Outcomes
Care management is another key element of JCMC’s valued-based care success. The multi-faceted program includes two dedicated care managers who focus on follow-up calls related to: all emergency room and hospital encounters, all “no show” office visits as part of preventive care, and all after-hours help line calls to assess the need for evaluation and an appointment with the primary care physician (PCP). In addition, the care managers identify community resources, with the goal of reducing or eliminating barriers to care. The care management program also coordinates with the care team to offer medication reconciliation to further identify patient needs and schedule follow-up PCP visits.
Another aspect of care management is care coordination, which is especially critical when patients need specialist referrals. JCMC leverages Infina Connect’s Intelligent Care Coordinator™ to give its PCPs the ability to direct patients to specialists within high value, virtual delivery networks when appropriate. This technology enables the exchange of clinical documents bi-directionally between disparate EHRs, ensuring collaborative care throughout the patient journey. By reducing referral leakage, JCMC further optimizes value-based reimbursement while delivering better care at a lower cost.
JCMC also utilizes Smartlink Health Solutions with SPH Analytics integration to take multiple, disparate data sources from EHRs, claims data and more, and bring it into the SPH Analytics engine to do risk stratification and identify care gaps, which are vital to population health management. Those care gaps are then pushed back into the EHR and care management system, empowering the physician and care managers with the right information at the right time within the clinical workflow.
Lastly, JCMC supplies its physicians with access to Smartlink Data Connector™, which automates the process of checking state prescription drug monitoring program (PDMP) databases, granting an informed prescribing decision while reducing administrative burdens. Checking the PDMP before prescribing opioids or controlled substances is required by North Carolina state law and is acknowledged as one of the most promising tools in identifying and preventing potential opioid abuse. The Smartlink solution automates the otherwise burdensome process of checking the state PDMP, making it easy for providers to comply with the law.
With its technology-driven care management system, complemented by the high-touch of its care managers, JCMC has improved clinical outcomes such as its enviable preventable hospital readmissions rate that is 75 percent below the regional average.
Overarching Cost Reduction
In addition to broadening patient access, engaging patients and integrating comprehensive care management, JCMC implemented other strategies that contributed to decreased costs and better care. First, the provider team prescribes generic drugs as a default, saving patients money with a therapeutically equivalent drug. Second, they minimize ancillary services, which means no in-house labs or X-rays, to reduce medically unnecessary usage. Third, they promote provider educational activities focused on value-based care and encourage provider engagement. Fourth, they continue their focus on preventive care and patient outreach with the primary care provider as the hub of the patient care wheel. All of these initiatives have resulted in a total cost of care that is 25 percent below the regional average.
Innovative Technology + Visionary Team = True Transformation
It’s no accident that we consistently rank high in numerous measures of cost and quality. We’ve done it by combining technology innovations with continuous process improvement, which has led to both lower cost and increasingly better care for our community.”
-Zen Menon, CEO of JCMC
JCMC had a vision for its path to value-based care. It involved collaborating with forward-thinking technology leaders, engaging its staff at all levels, and working together to create true transformation in healthcare. JCMC’s vision has been realized, as its providers deliver the highest quality care to their patients, at a lower cost and with higher revenue – a value-based care dream come true.
“It’s no accident that we consistently rank high in numerous measures of cost and quality,” said Menon. “We’ve done it by combining technology innovations with continuous process improvement, which has led to both lower costs and increasingly better care for our community. As a result, we’re well positioned to grow and thrive for years to come under value-based care.”


